|
|
A
32-year-old male surfer with a history of recurrent
childhood otitis media as well as adenoidectomy and
tympanostomy tube placement presents to the emergency
department with a complaint of progressive right ear pain
that started 2 weeks ago. Four days ago, he had seen an
otolaryngologist, who prescribed
ciprofloxacin-hydrocortisone ear drops for a diagnosis of
otitis externa. Two days after that, the patient was seen
in the emergency department because the pain worsened
despite treatment, and otitis externa was again diagnosed.
Acetaminophen-codeine was added to his regimen of ibuprofen
and the topical antibiotic. On this visit, he reports
having constant, severe ear pain and headache despite
analgesia. He denies having fever and vomiting but says he
cannot hear in his right ear. He denies any other medical
history, specifically a history of diabetes mellitus.
On physical examination, the patient appears well and has
normal vital signs. In his left ear canal are
moderate-sized canal exostoses; the left tympanic membrane
appears normal. For the right ear, the outer ear canal is
patent without notable narrowing, but a purulent,
yellow-gray discharge obscures the tympanic membrane and
inner canal. No substantial tenderness is noted with gentle
traction of the pinna or with compression of the tragus.
However, palpation of the temporal bone causes discomfort.
No obvious periauricular swelling or mass is observed. The
oropharynx is clear without trismus. No lymphadenopathy is
noted on neck examination. Neurologic examination reveals
no facial weakness, cranial nerve deficit, nystagmus, or
cerebellar findings. The rest of the physical examination
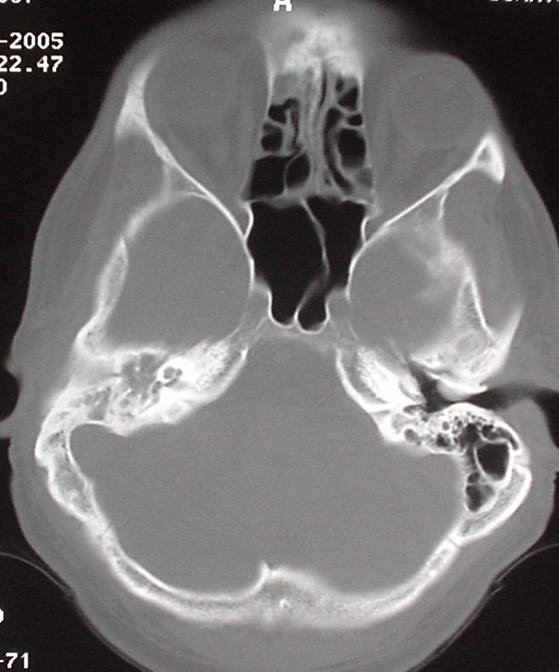
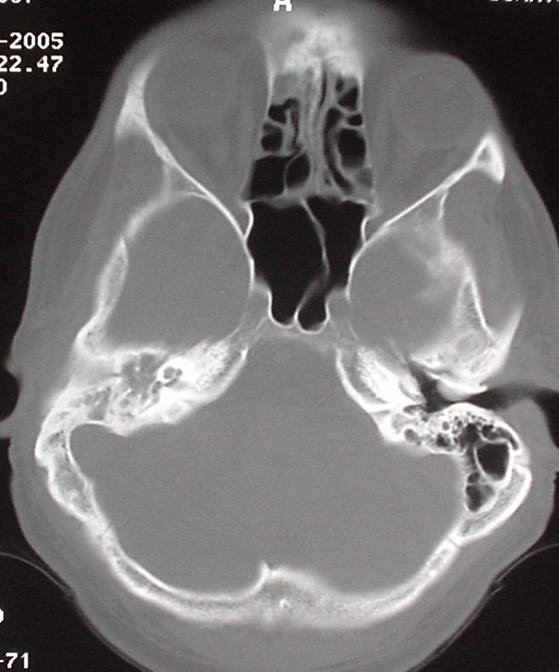
yields unremarkable findings. CT of the skull and brain is
performed (see Image).
What
is the diagnosis?
Answer
Mastoiditis: The CT scan demonstrates opacification
of the mastoid air cells on the right side
consistent with acute mastoiditis. Mastoiditis is a
rare complication of otitis media that has become
more infrequent since the advent of antibiotics. It
involves a local spread of infection into the
mastoid air cells in the temporal bone that
eventually causes bony destruction.
Clinical manifestations of mastoiditis include
decreased hearing, otalgia, otorrhea, tenderness,
and erythema and swelling over the mastoid process
that, when severe enough, may cause auricular
protrusion. The condition is most common among young
children, often in those who have had recurrent
acute otitis media. Although this condition was
classically thought to develop after prolonged acute
otitis media or after an asymptomatic period after
treatment, approximately one third of patients are
symptomatic for <48 hours before diagnosis. The
diagnosis is confirmed with CT, which demonstrates
opacification of mastoid air cells and destruction
of the bony cell walls.
Complications may include subperiosteal abscess,
meningoencephalitis, subdural empyema or abscess,
neck abscess (Bezold abscess), palsy of the seventh
cranial nerve (Gradenigo syndrome), labyrinthitis,
and venous sinus thrombosis. Organisms typically
found on culture to be responsible include Streptococcus
pneumoniae, Haemophilus influenza, and Streptococcus
viridans. Gram-negative bacteria may occur in
debilitated patients or patients with chronic
infections. The differential diagnosis of
mastoiditis includes otitis media, local cellulitis,
posterior auricular lymphadenopathy secondary to
local infection, and, in rare cases, rubella.
Treatment involves antibiotics, analgesics, and
often surgical drainage. About one half to two
thirds of patients respond to a 3- to 6-week course
of intravenous antibiotics alone. The rest
eventually require surgical intervention.
Broad-spectrum penicillins, such as
ampicillin-sulbactam or ticarcillin-clavulanate, are
the recommended primary agents. Alternative
antibiotics include second- or third-generation
cephalosporins. All patients with mastoiditis should
be admitted to the hospital for consultation with an
otolaryngologist.
|
Link
to further Information on:

For more information on mastoiditis, see the
eMedicine articles Mastoiditis
(within the Emergency Medicine specialty), Middle
Ear, Mastoiditis (within the Otolaryngology and
Facial Plastic Surgery specialty), and Mastoiditis
(within the Pediatrics specialty).
|
|





 DISCLAIMER:
This website is designed primarily for use by qualified
physicians and other medical professionals. The
information provided here is for educational and
informational purposes only. It is not guaranteed to be
correct and should NOT be considered as a substitute for
the advice of an appropriately qualified expert. In no way
should the information on this site be considered as
offering advice on patient care decisions or establishment
of a patient-physician relationship.
DISCLAIMER:
This website is designed primarily for use by qualified
physicians and other medical professionals. The
information provided here is for educational and
informational purposes only. It is not guaranteed to be
correct and should NOT be considered as a substitute for
the advice of an appropriately qualified expert. In no way
should the information on this site be considered as
offering advice on patient care decisions or establishment
of a patient-physician relationship.